This exercise program is not medical advice
Talk to your healthcare team about starting an exercise program before you begin.
This website should not be relied upon or serve as a replacement for medical advice from your healthcare team. Do not disregard or delay or discontinue your ongoing medical treatment because of your use of this website. Your continued treatment by your qualified medical practitioners is important to your health. If you have any concerns, address these with your medical team.
Any medical guidelines or recommendations from your medical practitioner regarding exercise in liver disease supersedes any information on this website. The information on the website is provided on an “as is” basis without any representations or warranties.
Balanced posture using light hand-held weights.
Aerobic
At this level, complete 150 minutes of moderate aerobic activity spread out over the week. For example, walk at a brisk pace or jog continuously for 30 minutes on 5 different days.
The goal is to reach and maintain between 3 to 5 on the Borg Scale – breathing stronger but can carry on a conversation.
Muscle strengthening
Aim to complete 3 to 4 sessions each week.
For each exercise, start with 2 sets of 10 repetitions each. Gradually increase to 3 sets of 15 repetitions.
Once this is achieved, increase the weight or resistance and begin anew with 2 sets of 10 repetitions.
While completing these exercises, aim to reach and maintain between 3 to 5 on the Borg Scale – breathing moderately but can still talk.
At P3, complete all 7 exercises listed. Allow 24 hours between each of these sessions so the muscles can recover. Can alternate between upper and lower exercise sessions if you wish to exercise every day.
Lateral Arm Raises with hand-held free weights
At P3, the weights should be more than 3 lbs each. Remember to increase the weight slowly to prevent injury.
(upper body)
Bicep Curl – single leg with hand-held free weights
(upper body)
Triceps Dip
Make sure to have someone holding the chair or support. Otherwise use an immovable support like a park bench or car/truck bumper. (upper body)
Leg Extension – with banding
Use a banding with a higher resistance than in P2. (lower body)
Leg Curls – with banding
Use a banding with a higher resistance than in P2. (lower body)
Calf Raises – with banding and single leg
Can use one or two legs . If using two legs, increasing the resistance of the banding. (lower body)
Squats – with hand-held free weights
At P3, the weights should be more than 3 lbs each. (include with either the upper or lower body exercise sessions)
Flexibility
Complete 1 set of 3 repetitions held for 20 to 30 seconds each. Hold the stretch until there is a slight discomfort. Avoid overstretching.
Perform at least two Flexibility sessions each week. These can be part of the cool down after a Muscle Strengthening session, combined with a Balance session, or completed on its own..
Include stretches from Intro (performed while standing) and P2.
Quad Stretch – seated
Balance
Complete 1 set of 10 steps with 3 repetitions at least twice a week. Increase the number of steps as you improve.
Make sure to have access to a wall or railing in case of unsteadiness.
A Balance session can be used as the cool down following a Muscle Strengthening session, can be combined with a Flexibility session, or completed on its own depending upon your schedule.
Heel-to-Toe Walk
Place the heel of one foot in front of the other so that the heal touches the toes. Now, walk in a straight line as far as you can go.
Example of a weekly P3 exercise program
Aerobic: Over 5 different days, complete 30 minutes of aerobic exercise for a weekly total of 150 minutes.
Muscle strengthening: On 3 or 4 days each week, do 2 sets of 10 repetitions of each of the following exercises:
- Lateral arm raises standing on one leg with hand-held free weights
- Arm curls with handheld free weights
- Overhead triceps extensions with hand-held free weights
- Leg extensions with banding
- Standing calf raises with banding
- Hamstring curl with a towel
- Squat with free weights
Flexibility: On 2 different days, perform all stretches 2-3 times lasting 20-30 seconds on each side.
Balance: On 2 different days, perform 3 repetitions of 10 steps each.
Lateral Arm Raise – single leg with hand-held free weights
Bicep Curl – single leg with hand-held free weights
Triceps Dip
Leg Extensions with banding
Leg Curls with banding
Calf Raises with banding and single leg
Squats with hand-held free weights
Useful Links
References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References:


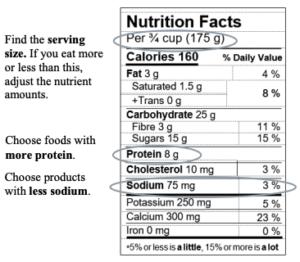
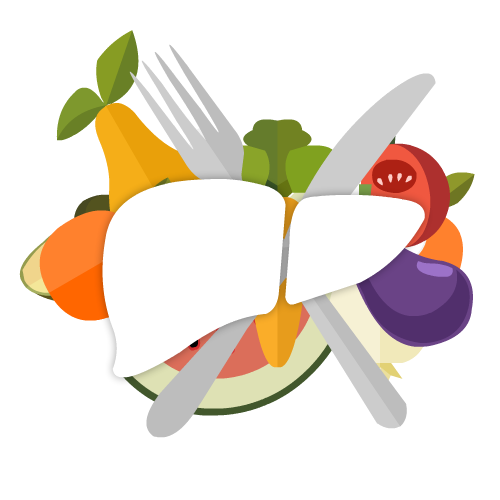
 Our national team of healthcare practitioners specializing in cirrhosis developed a practical “nutrition tool”
Our national team of healthcare practitioners specializing in cirrhosis developed a practical “nutrition tool”