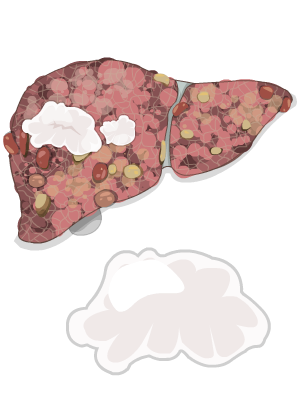
Liver Cancer or hepatocellular carcinoma, is a type of cancer that starts in the liver. It usually starts out as a small lump, called a tumor, and can grow larger over time. HCC (the short name for hepatocellular carcinoma) doesn’t start all of a sudden. It usually starts slowly in a liver that’s been exposed to risk factors for HCC.
Cirrhosis is, by far, the most important risk factor for HCC. In fact, HCC is rare in people without cirrhosis (except for those who have hepatitis B). It doesn’t matter what caused the cirrhosis—cirrhosis from any cause, is a significant risk factor for HCC.
Symptoms
In the early stage, HCC usually doesn’t cause any symptoms. This means that people can develop HCC and not know it right away. If left untreated, over time people with HCC might experience:
- Pain is in the right upper abdomen, which can travel to the right shoulder
- Swelling or fluid build-up in the abdomen
- Itchy or yellow skin if a tumor blocks the drainage of bile from the liver
- Nausea, vomiting, or poor appetite
- Weight changes
Diagnosis
Several tests are used to diagnose HCC. The most important ones are lab tests, physical examination, and imaging tests. In some cases, liver biopsies are also done.

Your doctor might also give you a physical exam. They’ll check your skin for signs of jaundice. They might feel your abdomen for lumps or a change in the size of your liver. They’ll also check for ascites, which is a buildup of fluid in the abdomen (belly).
Imaging tests are key to diagnosing HCC. HCC can usually be diagnosed solely by imaging tests such as ultrasound, MRI, and CT scan.
Ultrasound
An ultrasound of the abdomen is often the first imaging test that’s ordered. It can identify abnormal masses in the liver such as a tumor. It’s also used to screen for HCC in people who have a higher risk of developing the disease. High-risk patients usually get an ultrasound every 6 months to screen for HCC.
CEUS (Contrast Enhanced Ultrasound)
This is a type of ultrasound that uses microbubble contrast dye to look for tumprs in the liver. There’s no problem doing CEUS with poor renal function. CEUS is only available in a few highly specialized centres.
MRI
An MRI can provide more detail about blood vessels, organs, and lymph nodes. It’s useful for showing subtle differences in cells, and it can make it easier to see the liver and any tumors when there is fat in the liver.
When you get an MRI, you’re injected with a special dye called a contrast. If you have kidney problems or an allergy to iodine, the contrast dye most commonly used for MRIs might be safer for you than the one used for CT scans.
CT Scan
A CT scan combines a series of X-ray views taken from many angles to create a 3D image. It’s associated with a higher exposure to radiation.
CT scan images can provide much more information than plain X-rays. For HCC, a CT scan can show tumors and the blood vessels that the tumors might be growing into or around. A CT scan can also look at surrounding organs and check if the cancer is spreading into lymph nodes and other areas.
When you get a CT scan, you’re injected with a special dye called a contrast. The contrast dye makes the liver more visible.
A liver biopsy removes cells or tissues from your liver so they can be viewed under a microscope for signs of cancer.
A biopsy isn’t usually required to diagnose liver cancer. However, if the tumor doesn’t look like a typical HCC on a CT scan or MRI, a biopsy can be helpful to ensure the diagnosis is accurate prior to treatment.
Treatment
Your scans will be looked at, often by a specialized team that includes your liver specialist and other doctors with experience treating HCC. There are many things this team will consider when deciding which option to recommend for you…. things like:
- the size, number, and location of tumors
- your liver function (how well your liver’s working)
- your age and general health
Depending on your situation, some potential treatment options for HCC are:

- liver resection
- liver transplant
Liver Resection
If a liver tumor is small and hasn’t spread, your doctor might do surgery to remove the cancerous parts of the liver. This is called a liver resection. This operation is done only if you’re healthy enough for surgery and if all of the tumor can be removed while leaving enough healthy liver behind.
Cancerous parts of the liver that may be removed include:
- a small portion of tissue
- an entire lobe or even more
Before surgery, you’ll have imaging tests such as an MRI or CT scan to see if the cancer can be removed. Even with these kinds of tests, your doctor might discover during surgery that the cancer is too large or widespread to be removed. In this case, the partial resection is cancelled.
After surgery, risk of bleeding is a concern. Damage to the liver before and during the surgery can add to the potential bleeding problem. Other possible side effects include complications from anesthesia, blood clots, infections, and wound complications including hernias.
Also, the remaining liver still has the disease that led to the cancer (for example, cirrhosis). So there’s a chance that a new HCC can develop elsewhere in the liver after a partial resection.
Most liver resections are performed using an open technique, but some may be performed using a laparoscopic approach. The recovery time for surgeries varies from person to person. In general, these are the ranges:
| Type of Partial Resection | How Long in Hospital | Total Recovery Time |
|---|---|---|
| Open liver resection: performed through a fairly large incision |
5 to 10 days | 6 to 8 weeks |
| Laparoscopic liver resection: performed using a special scope, through 3 or 4 very short incisions | 3 to 5 days | 3 to 6 weeks |
Liver Transplant
In a liver transplant, the entire liver is removed and replaced with a healthy donated liver. A liver transplant will be considered when the cancer:
- is only in the liver
- can’t be treated as well by other standard treatment options
Usually only people with liver cancers up to a maximum size are candidates for a liver transplant. The precise size varies a bit from centre to centre. Your doctor will discuss transplant with you if it’s an option in your case.
With a transplant, the risk of a new HCC in the liver is reduced because all of the old liver is removed. There could, however, be a recurrence of the original cancer.
There are many things that will need to be consider aside from your HCC if you are being evaluated for liver transplant.
Targeted chemotherapy medications works differently from other chemotherapy because they attack a specific target—like cancer-related proteins—rather than attacking all body tissue. They often have different and less severe side effects.
Sorafenib
One example of a targeted chemotherapy medication for liver cancer is sorafenib. This medication is available as a pill. Sorafenib has been shown to stop the growth of cancer cells. It won’t cure liver cancer, but it can increase the lifespan of people who have this disease, typically for about 3 or 4 months.
Researchers are also studying the use of sorafenib in the early stages of liver cancer, often in combination with other kinds of treatment. They haven’t studied it much in people who have poor liver function, so it’s not known if it’s safe for these people.
Like other anticancer drugs, sorafenib has side effects including:
- diarrhea
- dry mouth
- dry or peeling skin
- itchiness
- rash, sometimes with blistering of hands and feet
- acne
- fatigue
- hair loss
- loss of appetite
- nausea and vomiting
- weight loss
Symptom management, is always part of treatment, but can be the main focus if other treatment options are not available
References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References:
