Top tips:
- Assess for and treat precipitants of HE
- Minimize/avoid opioids, sedatives and proton pump inhibitors
- Add Rifaximin with lactulose intolerance or with the second episode of overt HE. To date, the largest studies have evaluated the efficacy of Rifaximin in combination with lactulose.
- There is NO role for protein restriction in HE
- Do not order serum ammonia to diagnose or manage HE (Choosing Wisely Canada).
Navigation
General Cirrhosis Admission and Discharge Order Sets
*Add specific panels to general admission orders as appropriate*
For adults with cirrhosis requiring hospital admission
Cirrhosis Adult Admission Orders
For adults with cirrhosis requiring hospital discharge
Cirrhosis Adult Discharge Orders

Thank you to Dr. Bajaj for your efforts creating the content on this page!
Diagnosis and Immediate Management
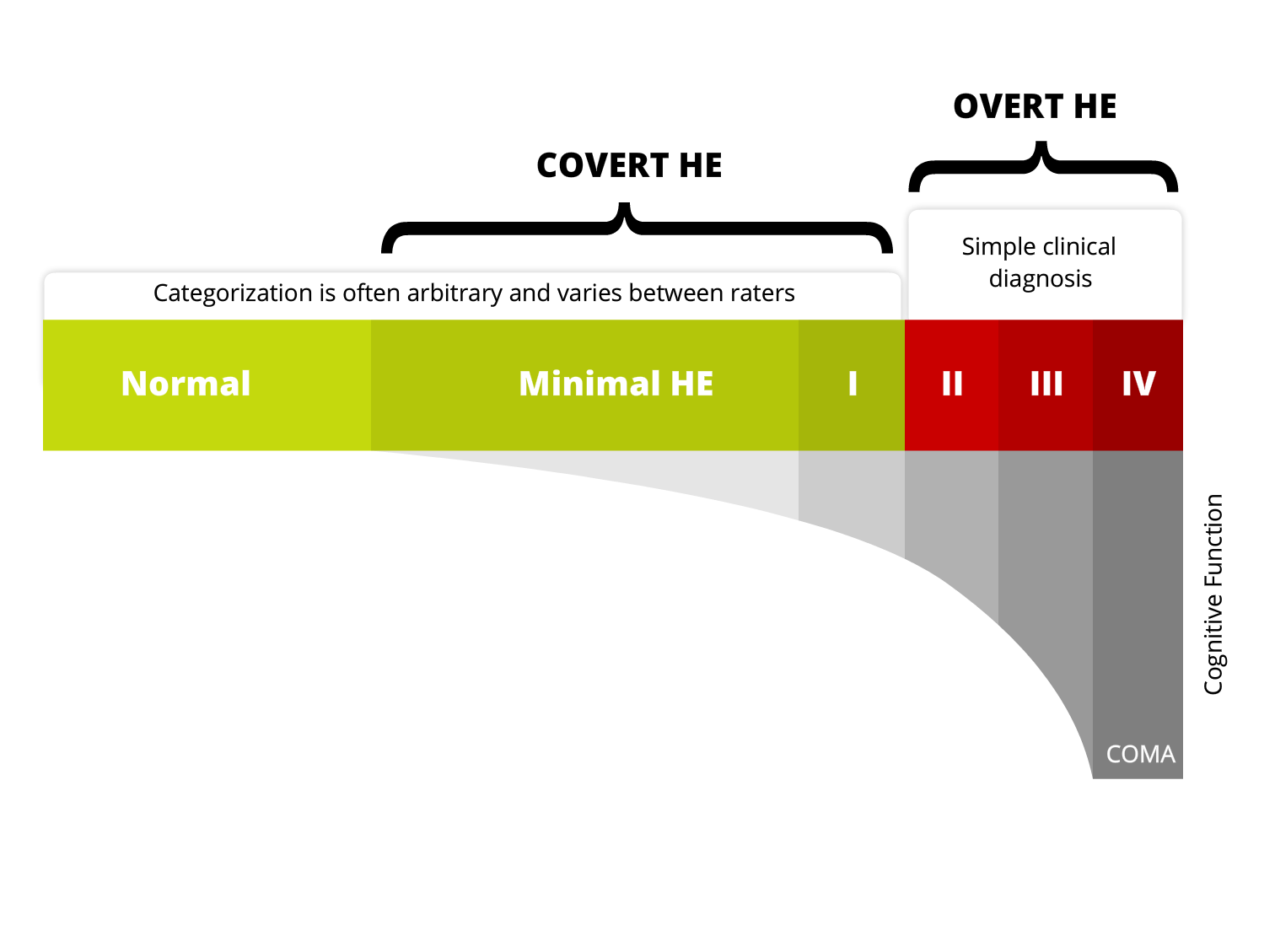
HE-Diagnosis-Immediate-Management-2Additional information on HE severity grading

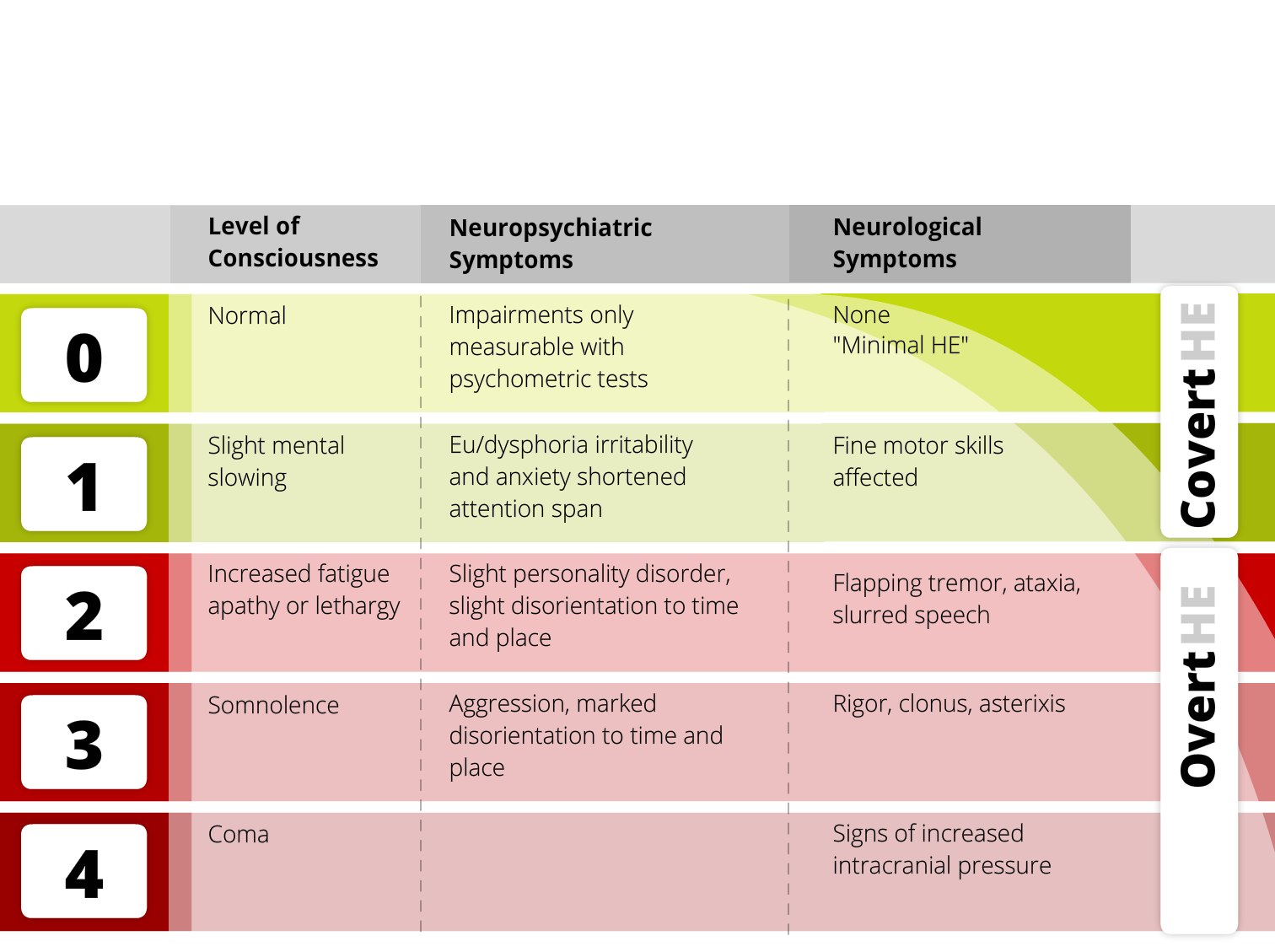
Clinical Hepatic Encephalopathy Staging Scale
(CHESS)
In order to assess clinical severity of hepatic encephalopathy, Ortiz et al. (Aliment Pharmacol Ther. 2007)
developed a scale initially composed of 48 items easy to categorize. Their analysis leads to the
establishment of a Clinical Hepatic Encephalopathy Staging Scale of nine items (CHESS), ranged
from normality (Hepatic Encephalopathy Clinical Staging Scale = 0) to deep coma (Clinical Hepatic
Encephalopathy Staging Scale = 9).
Identify and treat acute precipitants.
*Do not assume that HE is the result of noncompliance to lactulose before ruling out precipitants.
| Assess for: | |
|---|---|
 | Infection even if no clear signs on vitals or blood work: • Blood culture, urine culture and chest x-ray • Paracentesis if ascites |
| Constipation | |
| New medications (sedatives, narcotics) | |
| GI bleeding | |
| Metabolic abnormalities including renal injury, hypokalemia, hypovolemia, hypoxia. In some patients diuretics may be the only precipitant. |

| Medication | |
|---|---|
| Opioids | • Opioids can worsen HE due to sedation and constipation. • Minimize / wean with goal of stopping if possible. • Consider alternatives / adjuncts to pain management (i.e.) regular acetaminophen (can be used to maximum of 2000 mg per day) to help lower narcotic dosing. • Consider an extra lactulose dose per day with re-titration to 2-3 soft, formed bowel movements at initiation or increase of opioid/sedative medications. |
| GABAergics, sedatives and anxiolytics including benzodiazepines | • Minimize and avoid use if possible • Consider alternative therapy for the management of anxiety and depression |
| Proton pump inhibitors. | • There is an association between PPI use and Overt HE potentially related to alterations in the gut flora. • Reassess the indication for regular PPI use. Most people on PPI do not have a chronic need or indication. • If possible, dose reduce or stop the PPI. Start with reducing from twice daily dosing to daily to discontinuation if no return of symptoms. If return of GI symptoms, then consider intermittent PPI use at the lowest dose possible or a trial of a different drug class (e.g. H2 antagonists). |
Additional Management
HE-_additional_algPatient materials:
You can direct patients to the following:
Encephalopathy
Downloadable content:
You can download these to print or view offline:
AASLD Guidelines for HE
References:
This section was adapted from content using the following evidence based resources in combination with expert consensus. The presented information is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient’s care.
Authors: Dr. Matthew Sadler, Dr. Jasmohan Bajaj, Dr. Puneeta Tandon
References:
- EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol 2018 Aug;69(2):406-460 PMID 29653741
- Vilstrup H et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 2014 Aug;60(2):715-35 PMID 25042402
- Rahimi RS et al. Lactulose vs polyethylene glycol 3350–electrolyte solution for treatment of overt hepatic encephalopathy: the HELP randomized clinical trial. JAMA Intern Med 2014 Nov;174(11):1727-33 PMID 25243839
- Patidar KR, Bajaj JS. Covert and Overt Hepatic encephalopathy: Diagnosis and Management. Clin Gastroenterol Hepatol 2015 Nov; 13(12):2048-61 PMID 26164219
Last reviewed December 14, 2022.
