Top tips:
- Appetite loss and reduced caloric intake (anorexia) are common in cirrhosis
- Consider contributing causes and treat if appropriate according to goals of care.
- There is no robust cirrhosis specific data evaluating pharmacological therapy
- Refer to additional topics under the Healthy Living tab (malnutrition, frailty)
Anorexia is multifactorial, in part related to changes in pro-inflammatory upregulation and appetite mediators as liver disease progresses.
- Poor palatability of prescribed diets– e.g. dietary restriction of sodium ± other restrictions based on clinical diagnoses – see Nutrition section for patient resources. Depending upon the course of the patient’s disease, it may also be relevant to have discussions to understand the potential benefits (e.g. reduction in volume retention) versus burden (e.g. impact on quality of living, ability to enjoy or intake food) of continued sodium restriction.
- Early satiety, gastroparesis – medications, physical limitations such as ascites
- Dysgeusia (altered sense of taste) – zinc deficiency – test and treat
- Medications – culprits include antihistamines, opioids, certain antibiotics, antidepressants
- Hypogonadism – hypothyroidism, adrenal insufficiency, see sexual dysfunction page
A dietician consult and guidance can help evaluate and improve a patient’s nutrition.
Interdisciplinary consultation as appropriate – Dietitian, speech language pathologist, occupational therapist, physical therapist
- Food should be treated as medication- consider setting alarms as reminders to eat
- Smaller, more frequent high calorie meals and snacks (q3-4 hourly)
- Limit fluid intake when eating to reserve room for food
- Avoid drinks that reduce appetite and provide little nutrition such as coffee, tea and water
- Liquid nutritional supplements are useful high calorie liquid snacks
- Limit intake of spicy, acidic or overly sweet foods
- Cold foods may cause less aversion if nausea is an issue
Initiation of enteral supplementation can be discussed in concert with a Dietitian or Nutrition Specialist.
There is no data to support the routine use of appetite supplements in the setting of cirrhosis.
In cancer patients, appetite stimulants such as Megesterone acetate have not shown benefits on sarcopenia, physical function or survival. Use is associated with a risk of thrombosis.
At End of life, as the patient’s condition deteriorates, anorexia will worsen and it will not be amenable to therapy (including enteral/parenteral nutrition). Discussions around eating for pleasure may help patients to be able to balance adverse effects versus benefits at this stage. If anorexia or conversations around the utility of nutritional therapy at end of life are of particular distress for the patient, family or team, a consultation from Palliative Care should be obtained.
The Nutrition in Cirrhosis Guide
About the Guide
To download the complete "Nutrition in Cirrhosis Guide" (40 pages) as a .pdf file, click here.
The Guide was made possible from extensive feedback from patients, and their family & friends, who attend The Cirrhosis Care Clinic (TCCC) at the University of Alberta in Edmonton, Alberta, Canada.
This Guide covers general topics relevant to all patients with cirrhosis. Specific nutrition issues are also addressed that may be helpful at other times. The Guide is a tool for use throughout your cirrhosis journey.
The Guide is intended to be read a few pages at a time, beginning with those most important to your health or of interest to you.
The recipes (Chapter 4) are suitable for all individuals and can be modified to accommodate food allergies, dietary restrictions, and preferences.
Funding for the Guide’s creation was obtained from a research grant from the Canadian Institutes of Health Research (CIHR) and Alberta Innovates. Alberta Health Services provided protected time to V DenHeyer.

The following organizations provided support in the form of unrestricted educational grants to support the Guide:

Peer review regarding the content and format of the Guide was obtained from registered dietitians (RDs) and gastroenterologists in Halifax, Montreal, Toronto, Edmonton, Calgary, and Vancouver. Additional input was obtained from experts across North America and Europe. Thank you for your valuable input and assistance.
If any portion of the Guide is used in research, communications, or patient care, please use the following citation:
Tandon P, DenHeyer V, Ismond KP, Kowalczewski J, Raman M, Eslamparast T, Bémeur C, Rose C. The Nutrition in Cirrhosis Guide. University of Alberta, Edmonton, Alberta. 2018. pp. 1- 40.
The Nutrition in Cirrhosis Guide may be reproduced for non-commercial use as is and in its entirety without further permission. Adaptations, modifications, unofficial translations, and/or commercial use of The Nutrition in Cirrhosis Guide are strictly prohibited without prior permission.
The Cirrhosis Care Clinic
University of Alberta
Edmonton, AB, Canada T6G 2X8
www.wellnesstoolbox.ca
Clinician Primer

Click here to download the .pdf file (1 page)
This chapter covers the following topics:
-
Malnutrition risk profile for patients with cirrhosis
-
How & why the Guide will be helpful in your clinic
-
Who should read the Guide
-
Other patient-friendly websites providing helpful cirrhosis-specific information
-
References used in the creation of the Guide

Who will benefit from reading this chapter?
-
Physicians & Other Healthcare Practitioners providing care to patients with cirrhosis
-
Researchers
-
Any Patient with Cirrhosis
-
Anyone interested in the Guide
Chapter 1 – Malnutrition

Click to download the .pdf file (4 pages)
This chapter covers the following topics:
-
What is malnutrition?
-
Warning signs of malnutrition
-
Who is at-risk for malnutrition?
-
Why are patients with cirrhosis so susceptible?

Who will benefit from reading this chapter?
-
Any Patient with Cirrhosis
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Chapter 2 – What to eat and what to avoid?
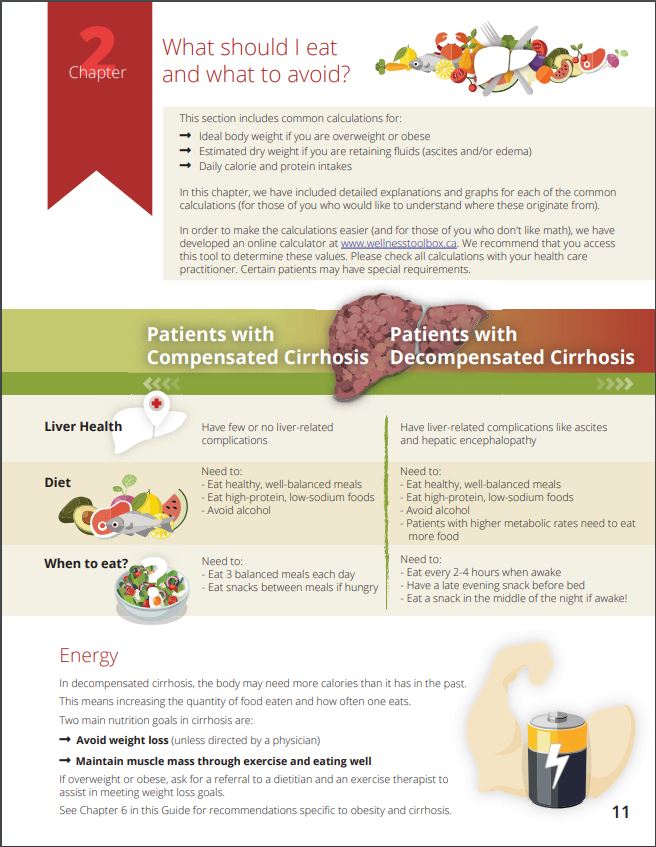 Click to download the .pdf file (14 pages)
Click to download the .pdf file (14 pages)
This chapter covers the following topics:
-
What foods to avoid eating? Which foods are good for the liver?
-
BMI Calculator (Body Mass Index)
-
Daily calorie intake - what is it and why it is important
-
Important nutrients: protein & sodium
-
How and why it's important to track body weight

Who will benefit from this chapter?
-
Any Patient with Cirrhosis
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Chapter 3 - Tips for eating even when not hungry

Click here to download the .pdf file (3 pages)
This chapter includes the following topics:
-
How to manage fatigue, cooking, and eating
-
How to cope when getting full after just a few bites
-
Smart tips for stretching the food budget
-
How to stick to a regular eating schedule
Who will benefit from reading this chapter?
-
Any Patient with Cirrhosis
-
Anyone who prepares food for person living with cirrhosis
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Chapter 4 – Recipes

Click here to download the .pdf file (4 pages)
This chapter includes liver-friendly recipes that are:
-
Nutritious
-
Easy to prepare & use inexpensive ingredients
-
Modifiable to accommodate dietary restrictions, tastes & preferences
-
Weight maintenance & weight loss friendly
-
Suitable for those with & without cirrhosis
Some recipe examples are:
-
Baked Chicken Dinner
-
Salmon Salad
-
Homemade Banana Muffins - YUM!
-
Black Bean Soup

Who will benefit from reading this chapter?
-
Anyone cooking for a Patient with Cirrhosis
-
Any Patient with Cirrhosis
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
-
Anyone looking for easy-to-make, nutritious & delicious recipes!
Chapter 5 – Meal supplements

Click here to download the .pdf file (2 pages)
This chapter includes topics about:
-
When are meal supplements useful?
-
Common meal supplement drinks
-
Which supplement drinks are best for which health conditions

Who will benefit from this chapter?
-
Any Patient with Cirrhosis with a poor appetite or needing snack ideas
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Chapter 6 - Managing weight loss & cirrhosis

Click here to download the .pdf file (3 pages)
This chapter includes sections on:
-
Diet priorities for non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH)
-
Protein intake - it's a priority!
-
Tips for reaching daily protein targets
-
Eating to help the liver & lose weight at the same time - Help?

Who will benefit from this chapter?
-
All Patients with NAFLD, NASH, or cirrhosis caused by NAFLD or NASH
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Chapter 7 - What to expect in the hospital

Click here to download the .pdf file (2 pages)
This chapter includes topics about:
-
What meals and snacks to expect
-
I can't follow my usual eating schedule - Help?
-
What is a "nasogastric (NG) feed"
-
Why an NG may be prescribed
Who will benefit from reading this chapter?
-
Any Patient with Cirrhosis who is being admitted to the hospital
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
To download the complete "Nutrition in Cirrhosis Guide" (40 pages) as a .pdf file, click here.
The Guide was made possible from extensive feedback from patients, and their family & friends, who attend The Cirrhosis Care Clinic (TCCC) at the University of Alberta in Edmonton, Alberta, Canada.
This Guide covers general topics relevant to all patients with cirrhosis. Specific nutrition issues are also addressed that may be helpful at other times. The Guide is a tool for use throughout your cirrhosis journey.
The Guide is intended to be read a few pages at a time, beginning with those most important to your health or of interest to you.
The recipes (Chapter 4) are suitable for all individuals and can be modified to accommodate food allergies, dietary restrictions, and preferences.
Funding for the Guide’s creation was obtained from a research grant from the Canadian Institutes of Health Research (CIHR) and Alberta Innovates. Alberta Health Services provided protected time to V DenHeyer.

The following organizations provided support in the form of unrestricted educational grants to support the Guide:

Peer review regarding the content and format of the Guide was obtained from registered dietitians (RDs) and gastroenterologists in Halifax, Montreal, Toronto, Edmonton, Calgary, and Vancouver. Additional input was obtained from experts across North America and Europe. Thank you for your valuable input and assistance.
If any portion of the Guide is used in research, communications, or patient care, please use the following citation:
Tandon P, DenHeyer V, Ismond KP, Kowalczewski J, Raman M, Eslamparast T, Bémeur C, Rose C. The Nutrition in Cirrhosis Guide. University of Alberta, Edmonton, Alberta. 2018. pp. 1- 40.
The Nutrition in Cirrhosis Guide may be reproduced for non-commercial use as is and in its entirety without further permission. Adaptations, modifications, unofficial translations, and/or commercial use of The Nutrition in Cirrhosis Guide are strictly prohibited without prior permission.
The Cirrhosis Care Clinic
University of Alberta
Edmonton, AB, Canada T6G 2X8
www.wellnesstoolbox.ca
Click here to download the .pdf file (1 page)
This chapter covers the following topics:
-
Malnutrition risk profile for patients with cirrhosis
-
How & why the Guide will be helpful in your clinic
-
Who should read the Guide
-
Other patient-friendly websites providing helpful cirrhosis-specific information
-
References used in the creation of the Guide
Who will benefit from reading this chapter?
-
Physicians & Other Healthcare Practitioners providing care to patients with cirrhosis
-
Researchers
-
Any Patient with Cirrhosis
-
Anyone interested in the Guide
Click to download the .pdf file (4 pages)
This chapter covers the following topics:
-
What is malnutrition?
-
Warning signs of malnutrition
-
Who is at-risk for malnutrition?
-
Why are patients with cirrhosis so susceptible?

Who will benefit from reading this chapter?
-
Any Patient with Cirrhosis
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
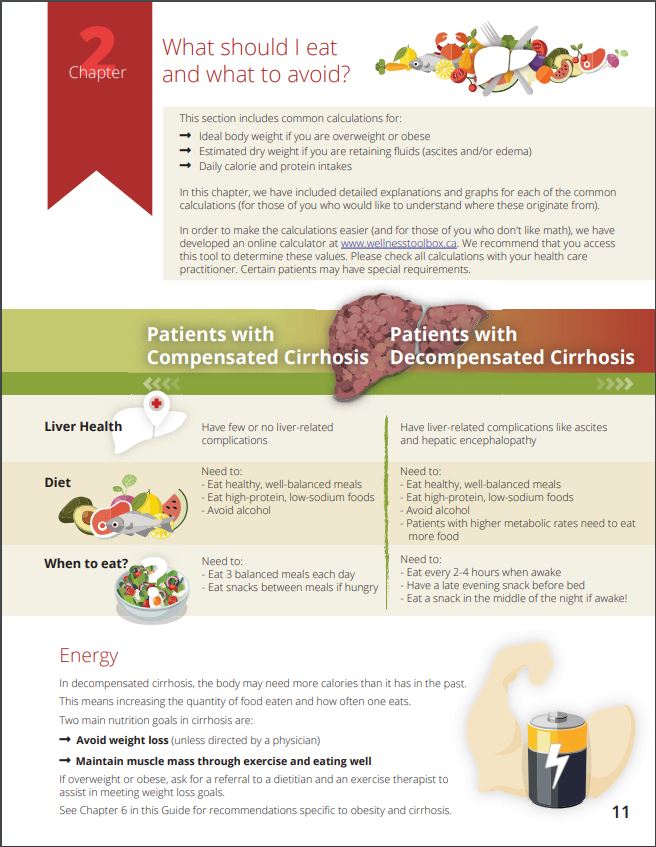 Click to download the .pdf file (14 pages)
Click to download the .pdf file (14 pages)
This chapter covers the following topics:
-
What foods to avoid eating? Which foods are good for the liver?
-
BMI Calculator (Body Mass Index)
-
Daily calorie intake - what is it and why it is important
-
Important nutrients: protein & sodium
-
How and why it's important to track body weight

Who will benefit from this chapter?
-
Any Patient with Cirrhosis
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Click here to download the .pdf file (3 pages)
This chapter includes the following topics:
-
How to manage fatigue, cooking, and eating
-
How to cope when getting full after just a few bites
-
Smart tips for stretching the food budget
-
How to stick to a regular eating schedule
Who will benefit from reading this chapter?
-
Any Patient with Cirrhosis
-
Anyone who prepares food for person living with cirrhosis
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Click here to download the .pdf file (4 pages)
This chapter includes liver-friendly recipes that are:
-
Nutritious
-
Easy to prepare & use inexpensive ingredients
-
Modifiable to accommodate dietary restrictions, tastes & preferences
-
Weight maintenance & weight loss friendly
-
Suitable for those with & without cirrhosis
Some recipe examples are:
-
Baked Chicken Dinner
-
Salmon Salad
-
Homemade Banana Muffins - YUM!
-
Black Bean Soup
Who will benefit from reading this chapter?
-
Anyone cooking for a Patient with Cirrhosis
-
Any Patient with Cirrhosis
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
-
Anyone looking for easy-to-make, nutritious & delicious recipes!
Click here to download the .pdf file (2 pages)
This chapter includes topics about:
-
When are meal supplements useful?
-
Common meal supplement drinks
-
Which supplement drinks are best for which health conditions

Who will benefit from this chapter?
-
Any Patient with Cirrhosis with a poor appetite or needing snack ideas
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
Click here to download the .pdf file (3 pages)
This chapter includes sections on:
-
Diet priorities for non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH)
-
Protein intake - it's a priority!
-
Tips for reaching daily protein targets
-
Eating to help the liver & lose weight at the same time - Help?

Who will benefit from this chapter?
-
All Patients with NAFLD, NASH, or cirrhosis caused by NAFLD or NASH
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners

Click here to download the .pdf file (2 pages)
This chapter includes topics about:
-
What meals and snacks to expect
-
I can't follow my usual eating schedule - Help?
-
What is a "nasogastric (NG) feed"
-
Why an NG may be prescribed
Who will benefit from reading this chapter?
-
Any Patient with Cirrhosis who is being admitted to the hospital
-
Caregivers
-
Family & Friends
-
Physicians & Other Healthcare Practitioners
This section was adapted from content using the following evidence based resources in combination with expert consensus. The presented information is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient’s care.
Authors (Alphabetical): Amanda Brisebois, Sarah Burton-Macleod, Ingrid DeKock , Martin Labrie, Noush Mirhosseini, Mino Mitri, Kinjal Patel, Aynharan Sinnarajah, Puneeta Tandon
Thank you to pharmacists Omer Ghutmy and Meghan Mior for their help with reviewing these pages.
References:
- Davison SN on behalf of the Kidney Supportive Care Research Group. Conservative Kidney Management Pathway; Available from: https//:www.CKMcare.com.
- Bruera E. ABC of palliative care. Anorexia, cachexia, and nutrition. BMJ. 1997 Nov 8;315(7117):1219-22. doi: 10.1136/bmj.315.7117.1219. PMID: 9393230; PMCID: PMC2127742.
- Bunchorntavakul C, Reddy KR. Review article: malnutrition/sarcopenia and frailty in patients with cirrhosis. Aliment Pharmacol Ther. 2020 Jan;51(1):64-77. doi: 10.1111/apt.15571. Epub 2019 Nov 8. PMID: 31701570.
- Ruiz-García V, López-Briz E, Carbonell-Sanchis R, Bort-Martí S, Gonzálvez-Perales JL. Megestrol acetate for cachexia-anorexia syndrome. A systematic review. J Cachexia Sarcopenia Muscle. 2018 Jun;9(3):444-452. doi: 10.1002/jcsm.12292. Epub 2018 Mar 14. PMID: 29542279; PMCID: PMC5989756