Top tips:
- In patients with risk factors for chronic liver disease AST, ALT and platelet count can help to rule out cirrhosis.
- A FIB 4 (calculated using age, AST, ALT and platelet count) cut-off score of < 1.3 is a good predictor of the ABSENCE of cirrhosis in all clinical contexts.
- As per the Alberta Health Services Fatty liver pathway (link), if your patient has a FIB-4 of more than or equal to 1.3, refer to a specialist trained in the management of liver disease.
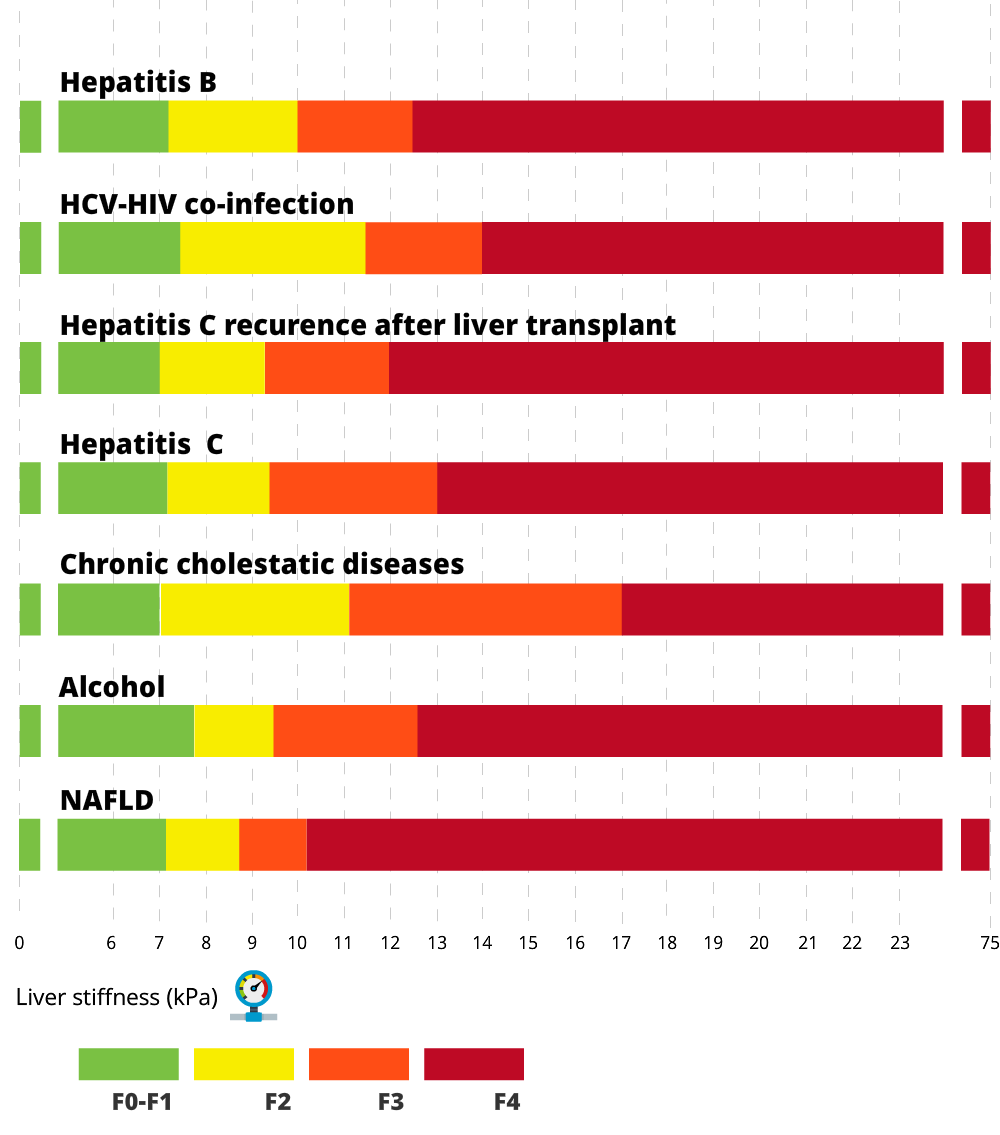
- Elastography is a good tool to assess liver fibrosis. Normal results of elastography can help to rule out cirrhosis and values over 15 kPa (by transient elastography) strongly suggest cirrhosis.
- A low platelet count (<150 G/L) is an important clue that a patient may have cirrhosis.
- Patients with suspicion of cirrhosis based on the above-mentioned tests should be referred to a liver clinic. Liver specialists will use clinical tools as well as a non-invasive approach based on liver Elastography and abdominal ultrasound to identify cirrhosis.
- In unclear cases, invasive tests (liver biopsy, hepatic venous pressure gradient measurement, endoscopy) will be required to come to a final diagnosis.


Check out the bottom of the page for short videos from Dr. Abraldes and Dr. Berzigotti!

Spider Nevus
Images courtesy of Patrick Kamath, MD
- Dilated arterioles characterized by prominent central arteriole and radiating vessels, usually found in distribution of superior vena cava
- Compression of central arteriole causes blanching of the “spider”
- More than 3 spider nevi is considered abnormal
Palmar Erythema
Image courtesy of Patrick Kamath, MD
- Intense red coloration of the thenar and hypothenar eminence
Terry Nails
Image courtesy of Patrick Kamath, MD
- Characterized by proximal nail bed pallor
- Can also involve the entire nail plate
- Predominant involvement of the thumb and index finger
Clubbing
Image courtesy of Patrick Kamath, MD
- Associated with hepatopulmonary syndrome
Gynecomastia
Image courtesy of Patrick Kamath, MD
- Enlargement of male breasts with palpable tissue
Caput Medusae and Ascites

Image courtesy of Patrick Kamath, MD
Image courtesy of Dr. A Berzigotti
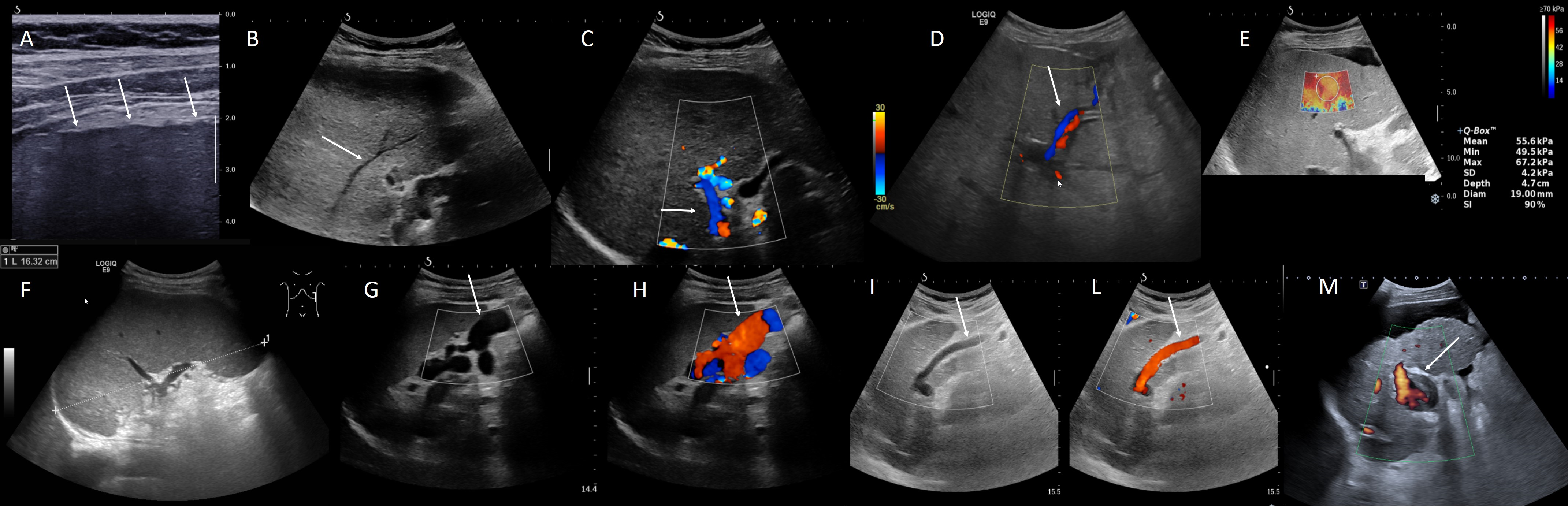
Figure summarizing the most common ultrasound findings in patients with cirrhosis
A) Nodular liver surface (arrows)
B) Liver vein with a reduced diameter and irregular walls due to the compression of the surrounding cirrhotic parenchyma. Heterogeneous parenchyma
C) Hepatofugal (away from the liver) blood flow in the portal vein. This finding suggests very high resistance in the liver and lower resistance outside the liver, usually due to the presence of large porto-systemic collaterals
D) Left intrahepatic branch of the portal vein shows hepatofugal blood flow
E) 2D-Shear Wave Elastography shows very high liver stiffness values (> 55 kPa). Small amount of ascites around the liver surface
F) Enlargement of the spleen quantified by ultrasound by measuring the pole to pole distance. Here is 16 cm (severe splenomegaly)
G) Porto-systemic collaterals close to the spleen appear as large anechoic channels
H) By using color-Doppler, the channels show venous flow in the direction of the renal vein, confirming the diagnosis of spleno-renal collaterals
I) In the left lobe (sagittal view) a long channel can be often observed between the left portal vein and the extrahepatic space, within the ligamentum rotondum. This corresponds to a patent paraumbilical vein
L) The diagnosis can be confirmed by using color-Doppler, which shows hepatofugal flow within this vessel
M) Advanced cirrhosis: small liver, with nodular surface and heterogeneous parenchyma. The portal vein is dilated, and 50% of the lumen is occupied by echogenic material, confirming the diagnosis of portal vein thrombosis. The liver is surrounded by ascites
Patient should be fasting for at least 2 hours
Quality criteria:
- Need 10 Valid shots
- Need >60% success rate = valid shots/total shots
- Need IQR (Interquartile range)/M (median liver stiffness measurements) ≤ 0.3
Consider the following parameters that may impact interpretation:
- Serum aminotransferases ≥ 5 x ULN
- BMI (use XL probe if BMI >30 kg/m2 or skin-to-capsule distance >25 mm)
- Extra-hepatic cholestasis
- Right heart failure or other causes of congestive liver
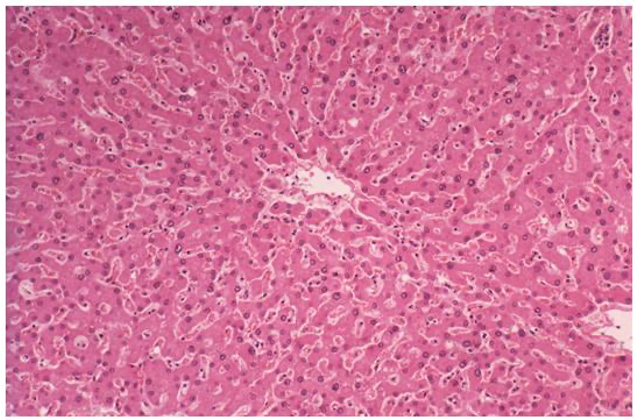
Normal
Image courtesy of Patrick Kamath, MD
In the normal liver, plates of hepatocytes are arranged in a concentric fashion around the portal tract (blue curved arrow)
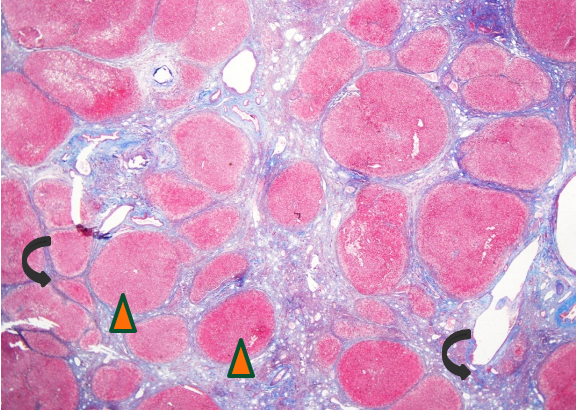
Cirrhosis
Image courtesy of Patrick Kamath, MD
In cirrhosis, the normal hepatic architecture is replaced by diffuse fibrosis (black curved arrows) with nodular regeneration (arrowheads)
Introducing Dr. Abraldes and Dr. Berzigotti

Patient materials:
You can direct patients to the following:
What the liver does
: Links and Calculators
Alberta Health Services link to the fatty liver pathway
Use these calculators to help with the diagnosis:
APRI
Downloadable content:
You can download these to print or view offline:
EASL Guidelines
Video Links:
See relevant videos:
FibroScan user tutorial-short version
References:
This section was adapted from content using the following evidence based resources in combination with expert consensus. The presented information is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient’s care.
Authors: Dr. Mang Ma, Dr. Annalisa Berzigotti, Dr. Puneeta Tandon
References:
- EASL-ALEH Clinical Practice Guidelines: Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol 2015 Jul;63(1):237-64 PMID 25911335
- Kelly EMM et al. An Assessment of the Clinical Accuracy of Ultrasound in Diagnosing Cirrhosis in the Absence of Portal Hypertension. Gastroenterology and Hepatology 2018 Jun; 14(6):367-373 PMID 30166950
Last updated November 10, 2022.