Top tips:
- Advanced care planning is an iterative and longitudinal process of patient-centered medical decision-making that is guided by patients’ personal goals, values, and current health circumstances to elicit their goals and preferences for medical care
- Identifying, documenting, and preparing surrogate decision-makers early in the disease course is a key component of advance care planning in cirrhosis care prior to patients losing capacity
- Goals of care should be reassessed regularly during routine care but especially after sentinel events such as new clinical deteriorations or acute changes in health status or home/social circumstances
- Anticipatory guidance for medical decision-making should include an assessment of preferences for future treatment options (e.g. endoscopic procedures, renal replacement therapy, mechanical ventilation, cardiopulmonary resuscitation) and place of care in the event of progressive or terminal illness



Thank you to Dr. Woodrell, Dr. Patel, and Dr. Ufere for your efforts creating the content on this page!
Figure 1. The ACP Process and Key Elements

Figure 1. The ACP process in cirrhosis care. Adapted [reprinted] from “Advance care planning (ACP) for specialists managing cirrhosis: A focus on patient-centered care,” by Amanda Brisebois, Kathleen P. Ismond, Michelle Carbonneau, Jan Kowalczewski, and Puneeta Tandon, 2017, Hepatology, 67(5). Copyright year 2018 by All Authors.
Talking points:
- Assessing goals/values/perspectives
- Assessing readiness
- Early identification and documentation of surrogate decision-maker
- Preparation of surrogate decision-maker
- Caregiver focused website
-
- Cirrhosis education
- Discussing prognosis
- Reviewing cirrhosis complications
- Document GOC including preferences for future medical care and place of care
When to initiate ACP discussions for patients with cirrhosis
Table 1. Suggested Clinical Milestones and Life Events That Should Trigger ACP Discussions for Patients with Advanced Liver Disease
| Liver-Specific Factors | Patient Factors | Major Life Events |
|---|---|---|
| New liver-related complications (ascites, hepatic encephalopathy, variceal bleeding, hepatocellular carcinoma) | Advanced multimorbidity | Recent ICU admission |
| New diagnosis of refractory ascites | Poor performance status and/or progressive frailty | Recent unplanned hospitalization for a liver-related complication |
| New diagnosis of acute kidney injury or hepatorenal syndrome | Ongoing substance use disorder | Loss of a spouse or primary caregiver |
| Recently delisted or declined for liver transplantation | New comorbid diagnosis of cancer, cardiovascular disease, neurological disease, or other life-limiting condition | Advanced age |
Note. Reprinted [adapted] from “Advance Care Planning and Goals of Care Discussions in Advanced Liver Disease,” by Nneka N. Ufere, 2021, Current Hepatology Reports, 20, 77. 2021 by Author(s).
How to initiate ACP discussions for patients with cirrhosis

| Topics | Conversation Starters |
|---|---|
| Patient perspectives | Level of detail —Are you a detail-oriented learner or do you prefer a general overview and plan?Learning style —Some people are visual leaners while others process conversations best. Which learning approach suits you the best? Values and fears —What is most important to you in life? —What aspect of health would need to be taken from you, for you to feel that living was worse than dying? |
| Education | —Meeting for the first time about a new illness that you have been diagnosed with can be overwhelming —We have created educational pamphlets we can provide for you, which can help guide our future discussions. —Our clinic communicates with your other health providers, so that we all know your wishes and details regarding your health |
| Readiness | Readiness to discuss ACP and GCD —Very ill patients with cirrhosis cannot always make their own health care decisions. We like to talk about these things early on to understand what you value in case such a situation arises. How would you feel discussing how cirrhosis may affect you in the future? Readiness to choose a surrogate —If you were to get very sick, is there anyone you trust to make medical decisions for you? Does this person know what is important to you? |
| Focus of care | —Recently, you had a complication of cirrhosis and were quite unwell. I would like to explain how cirrhosis may affect you in the future. —It is important to understand how disease-modifying treatments and symptom control therapies are used together an illness. |
| Prognosis | Discuss in general terms —To make sure that both you and your family are prepared, I like to address both the best-and worst-case scenarios regarding how your cirrhosis may progress. Can we talk about these now? —Some patients ask me how their cirrhosis will affect how long they live. Are you interested in this type of information? |
| Review cirrhosis | Disease complications —The investigations that we have done show that your disease has worsened. I would like to discuss how that affects what treatments and therapies are going to help you live the best-quality of life possible End-of-life wishes —What would be important to you in your last months of life? —Where would you prefer to die? |
| Resources | —Many communities have additional supports for patients with medical, social, psychological, and spiritual needs. Would you be interested in learning about some of these resources? |
| Documentation | —This depends on where patient is located. Various websites describe local and regional Goals of Care Medical Orders. — In Alberta, Canada, Conversations Matter describes local requirements |
| Review and compare | —Please tell me what you understand of your decisions with respect to your GCD. What impact do they have on your life? I want ot ensure that the designation properly reflects your values and wishes —Since we last met, have you had any experiences that may change your view about living with cirrhosis? — Are your wishes outlined anywhere else, such as in a Will or legal document? If so, we should look at it to ensure your wishes are consistent with your medical documents |
| Setting | Setting up the interview •Arrange for some privacy •Involve significant others if the patient chooses •Invite other relevant parties: Interpreter, social worker, surgeon, palliative care physician •Sit down with the patient •Make a connection and establish rapport with the patient •Manage time constraints and interruptions |
| Perception | Assessing the patient's perception •Use open-ended questions to determine the patient's level of comprehension about his or her medical condition (i.e. "What have you been told about your medical situation so far?") |
| Invitation | Obtaining the patient's invitation •Assess the patient's readiness to receive information •Discuss information disclosure at the time of ordering studies (i.e. "I have some updates on your condition to discuss. Would it be all right if I share these with you now?") •If the patient does not want to know details, offer to answer any questions they may have in the future or to talk to a caregiver |
| Knowledge | Giving knowledge and information to the patient •Consider a warning prior to disclosing bad news to the patient (i.e. "Unfortunately, I do not have good news" or "I'm sorry to tell you that...") •Start at the level of comprehension and vocabulary of the patient •Try to use nontechnical words and avoid medical jargon •Avoid excessive bluntness •Give information in small chunks, and periodically reassess the patient's understanding •When the prognosis is poor, avoid using phrases such as "There is nothing we can do for you" as patients may have other important therapeutic goals outside of curative therapy such as good symptom relief |
| Emotion | Addressing the patient's emotions with empathic responses •Observe for any emotion on the part of the patient •Identify the emotion experienced by the patient by naming it to oneself-use open ended questions to query the patient as to what they are feeling •Identify the reason for the emotion - if you are not sure, ask the patient •After you have given the patient time to express his or her feelings, show the patient that you recognize and empathize with his or her emotional response |
| Strategy and Summarize | Presenting a clear plan for the future with the patient •Assess whether the patient needs clarification on what has been discussed •Ask the patient if he or she is ready for a discussion regarding next steps in management •Set out a medical plan of action |
Adapted from Baile et al, Oncologist 2000
Physician communication skills training
Patient facing educational tools
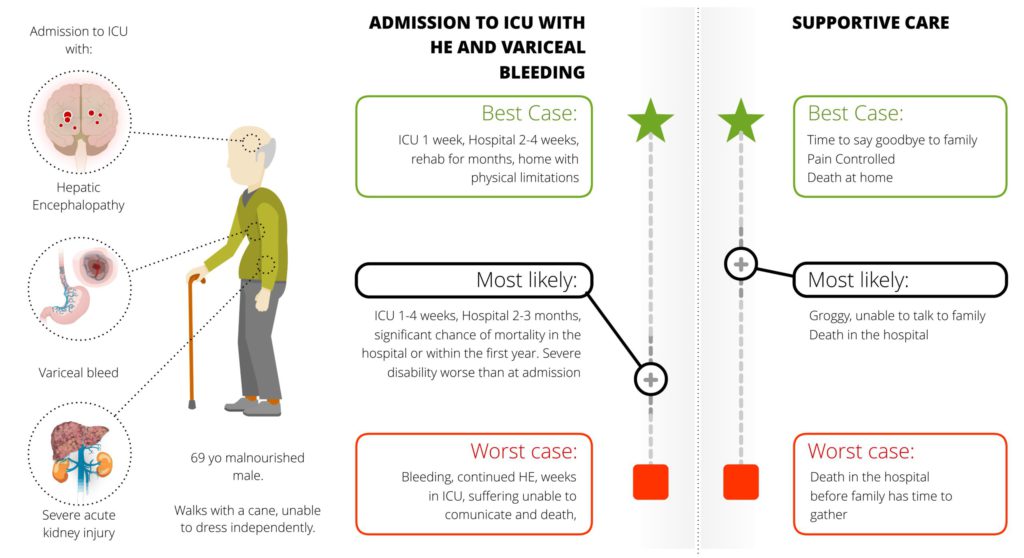
Best Case/Worst Case Tool

Optimizing outpatient processes for ACP


- Health care professionals who may furnish and bill ACP: Physicians, clinical nurse specialist, nurse practitioners, physician assistants
- Since ACP services are voluntary, Medicare beneficiaries (or their legal proxies when applicable) should be given a clear opportunity to decline to receive ACP services. Beneficiaries, family members and/or surrogates may receive assistance for completing legal documents from others outside the scope of the Medicare program in addition to, or separately from, the physician or NPP.
- Examples of appropriate documentation would include an account of the discussion with the beneficiary (or family members and/or surrogate) regarding the voluntary nature of the encounter; documentation indicating the explanation of advance directives (along with completion of those forms, when performed); who was present; and the time spent in the face-to-face encounter
- To bill for advance care planning services provided during an Evaluation and Management (E/M) office visit or inpatient consult/follow-up visit, providers can use the modifier code 25 and the following ACP codes as follows:
- CPT Code 99497: Can be used to bill for advance care planning performed by a qualified health care professional for the first 30 minutes (minimum of 16 minutes) spent face-to-face with the patient, family member(s), and/or surrogate. This includes the explanation and discussion of advance directives such as health care proxy or MOLST forms. This include, but does not require, the completion of such forms.
- CPT Code 99498: Can be used for each additional 30 minutes (minimum of 16 minutes past the first 30 minutes documented) of advance care planning performed by a qualified health professional. List separately in addition to code for primary procedure
- Visits that are dedicated to ACP alone may also be billed separately using CPT codes 99497 and 99498
Patient materials:
You can direct patients to the following:
Personal Directive
Power of Attorney
Living Wills
Patient Educational Brochures
Helpful Links:
Advance care planning kit
Cirrhosis Care: Advance care planning kit
Select Improvement Solution: ACP
Conversations Matter
Plan well guide
AASLD End of life planning
AGA Clinical Practice Update on Palliative Care Management in Cirrhosis
Communication Trainings:
Vital Talk
Serious Illness Conversation Guide
Caregiver Centered Care
References:
This section was adapted from content using the following evidence-based resources in combination with expert consensus. The presented information is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient’s care.
Authors: Dr. Nneka Ufere, Dr. Arpan Patel, Dr. Christopher Woodrell, Dr. Amanda Brisebois, Dr. Rebecca Sudore, Dr. Puneeta Tandon
References:
-
- Tandon P, Walling A, Patton H, Taddei T. AGA Clinical Practice Update on Palliative Care Management in Cirrhosis: Expert Review. Clinical Gastroenterology and Hepatology. 2021;19(4):646-656.e3. doi:10.1016/j.cgh.2020.11.027. PMID 33221550
- Brisebois A, Ismond KP, Carbonneau M, Kowalczewski J, Tandon P. Advance care planning (ACP) for specialists managing cirrhosis: A focus on patient-centered care. Hepatology. 2018;67(5):2025-2040. doi:10.1002/hep.29731.PMID 29251778
- Ufere NN. Advance Care Planning and Goals of Care Discussions in Advanced Liver Disease. Current Hepatology Reports. 2021;20(3):77-84. doi:10.1007/s11901-021-00565-x.
- Baile, W. F., Buckman, R., Lenzi, R., Glober, G., Beale, E. A., & Kudelka, A. P. (2000). SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. The oncologist, 5(4), 302–311. https://doi.org/10.1634/theoncologist.5-4-302PMID 10964998
