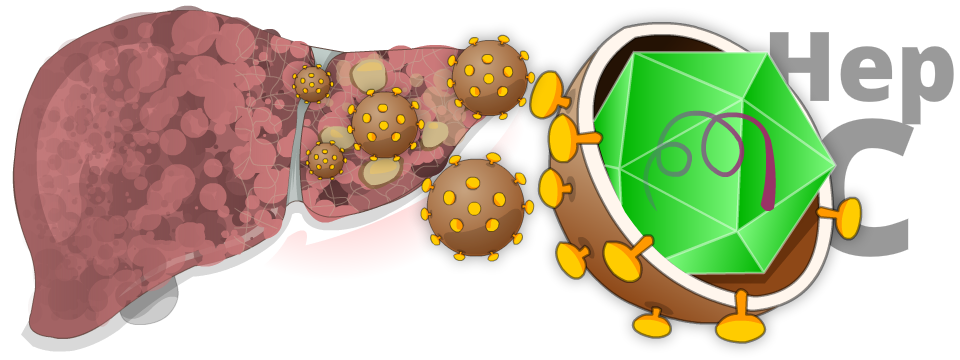
Hepatitis C is a contagious virus that can cause liver disease liver disease. it is sometimes called HCV for short.
Hepatitis means inflammation of the liver. When the liver’s inflamed (swollen and irritated), it has a harder time functioning properly. When this happens for a prolonged time, the liver starts to lose its ability to function, and a person may get sick.
Some people who get infected with hepatitis C never feel sick and recover completely. Others develop acute or chronic hepatitis C.
Risk Factors

- You received a blood transfusion, blood products, or an organ transplant before July 1990 in Canada
- You’ve been in jail
- You use or have used injection drugs, even if it was just once or many years ago
- You’ve been injected or scratched during vaccination, surgery, blood transfusion, or a religious/ceremonial ritual in regions where hepatitis C is common
- Having a sex partner infected with hepatitis C (low risk)
- Born to a mother infected with hepatitis C
- Manicures or pedicures with improperly sterilized equipment
- Tattoos or body piercing
- Traumatic or rough sex or sex toys that can tear body tissue
- Vaginal sex during menstruation
- Multiple sex partners
- Having a sexually transmitted infection (STI) such as lymphogranuloma venereum (LGV)
- Medical procedures with improperly sterilized equipment
- You’ve had kidney treatment (hemodialysis)
- You’ve had an injury from a needle
- Sharing cocaine (snorting) equipment
- Sharing personal hygiene items with an infected person such as nail clippers, razors, or toothbrushes
- You have another infectious disease such as hepatitis B or HIV
- Breastfeeding (unless your nipples are cracked and bleeding)
- Coughing or sneezing
- Hugging and kissing or other casual contact
- Oral sex (unless blood is present)
- Sharing food, drinks, or eating utensils
- Touching or shaking hands
- Using toilet seats
Symptoms
The symptoms of hepatitis C are often mild. Most people carry the virus for years and don’t notice any symptoms. When they do notice symptoms, the most common ones are:
- “brain fog” (the sense that you’re not thinking and concentrating normally)
- fatigue
- joint pain
- loss of appetite
- weight loss
Diagnosis
You don’t need a liver biopsy to determine if you have hepatitis C. Usually, two lab tests are used to diagnose it: hepatitis C antibody (Anti-HCV) and hepatitis C RNA (HCV RNA).
Hepatitis C Antibody (Anti-HCV)
This is the first hepatitis C test your healthcare providers will perform. It will find out if your body has antibodies against hepatitis C. A positive result means that at some point in your life, you were exposed to the hepatitis C virus, and you developed antibodies to it. But it doesn’t tell us if you’re still infected. So, if this test is positive, your healthcare providers will perform the hepatitis C RNA (HCV RNA) test to find out if you’re still infected.
Hepatitis C RNA (HCV RNA)
The hepatitis C RNA (HCV RNA) test will be used to find out if you still have the virus in your body. If the HCV RNA test is positive, you have chronic hepatitis C and should be considered for treatment to clear it.
Genotypes
Hepatitis C genotypes are different strains of the hepatitis C virus. There are six genotypes around the world. In Canada, the more common genotypes are 1, 2, and 3. Genotypes matter very little now, because the newer treatments are effective against all genotypes. In many jurisdictions, genotypes are no longer tested or reported.
Treatment
Since 2010, the medical community has made enormous progress in treating chronic hepatitis C. New medications called direct-acting antivirals (DAAs) act on the virus itself to rid it from the body. This is different than older medications like interferon, which works by stimulating an immune response.
These newer treatments are very effective and have cure rates of over 95%. Interferon is no longer used for hepatitis C treatment.
The newer treatments take less time (between 8 to 12 weeks), have fewer side effects, and appear to be effective at all stages of the disease.
Because these treatments are newer, they’re still expensive. But the cost is generally covered by provincial drug benefit programs or private insurance companies. Virtually all patients in Canada can now access these life-saving treatments that cure hepatitis C.
Alternative Therapies
If you’re trying alternative therapies such as herbal remedies, homeopathic medicines, and minerals, tell your healthcare providers. Please note: no alternative therapies have been proven safe and effective for clearing (curing) hepatitis C.
Q&A

Yes. Although your body’s immune system makes antibodies to fight hepatitis C, these antibodies don’t fully protect you. The virus changes so quickly that it can escape your body’s defenses. This means that you can’t have lifelong protection from hepatitis C, and this is the reason why there’s no current vaccine for hepatitis C available. If you’re treated for hepatitis C and get rid of the virus, you can still be infected again. Therefore, what you do—or don’t do—can affect your level of risk for getting hepatitis C again.
Some people clear their body of the virus on their own in the weeks after they’re infected. But most people who get hepatitis C develop a chronic infection.
When a chronic infection occurs, the hepatitis C virus multiplies in the liver. Parts of the virus trigger the immune system into action. While trying to rid the body of the infection, the immune system kills infected liver cells.
Chronic hepatitis C progresses slowly over 10 to 40 years. But for some people, the interaction between their immune system and liver can result in scarring of the liver (fibrosis or cirrhosis) and loss of liver function.
Statistics on Outcomes of Hepatitis C
Someone with hepatitis C has a 20% chance that their liver scarring will progress from fibrosis to cirrhosis in the first 20 years. Alcohol markedly increases this risk. A heavy drinker with hepatitis C has many times the risk of developing cirrhosis compared to a non-drinker with hepatitis C. Alcohol and hepatitis C both damage the liver. Together, the risk of serious liver damage is much higher than either alone.
If you have hepatitis C, you can give the virus to other people. This is true even if you feel fine. To protect others from getting hepatitis C, follow these suggestions:
- Don’t donate blood, body organs, tissues, or sperm.
- Don’t let anyone else use your razor, toothbrush, or other personal care items.
- Cover open cuts or sores on your skin with a bandage until they’re healed.
- Don’t inject drugs. If you’re injecting drugs, talk with your healthcare provider about trying to stop, and call the Alberta Addiction Helpline at 1-866-332-2322 for help. If you don’t stop, never share your needles, or works (cotton, cooker, spoon, etc.) with anyone else.
- Practice safer sex. Use a latex barrier, such as a condom, every time you have sex. Using condoms also reduces your chances of getting sexually transmitted infections (STIs).
Following these suggestions can also protect you from other diseases such as hepatitis B and HIV.
References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References:
