Hepatitis means inflammation of the liver. When the liver’s inflamed (swollen and irritated), it has a harder time functioning properly.
Hepatitis viruses cause inflammation. There are different types of hepatitis viruses such as hepatitis B and C. Other hepatitis viruses such as hepatitis A and E may cause serious inflammation of the liver, but they resolve on their own in most cases and don’t lead to cirrhosis.
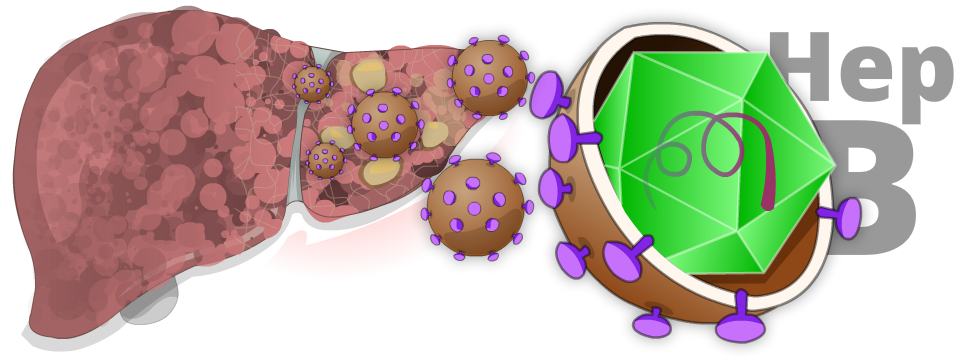
Hepatitis B is a contagious liver disease that results from infection with the hepatitis B virus. It’s common worldwide. In regions where hepatitis B is most common, such as countries in Asia and Africa, at least one in five people may be infected with the virus.
Hepatitis B ranges in severity and can be either acute or chronic.
| Acute Hepatitis B | Chronic Hepatitis B |
|---|---|
| A mild, short-term illness lasting a few weeks. | A serious, long-term, lifelong illness. |
| Happens within the first 6 months after someone is exposed to the virus. | Occurs when the virus stays in a person’s body. |
| Acute infection can—but doesn’t always—lead to chronic infection (chronic hepatitis B). | The younger people are when they’re infected with the hepatitis B virus, the greater their chance of developing chronic hepatitis B. |
Causes
The hepatitis B virus is not in food or water. It’s in blood and other body fluids, and it’s contagious. It passes from person to person when blood, semen, or other body fluid infected with the virus enters the body of a person who’s not infected.
In North America, the vast majority of people with chronic hepatitis B have immigrated from an area where it’s common, such as Asia and Africa, and they were infected at birth.
Adults who get hepatitis B, usually through sex, will clear the infection themselves in about 99% of cases. Therefore, they will have only acute hepatitis B—not chronic—and will not have long-term health problems.
| Hepatitis B is Not Passed By | Hepatitis B Can Be Passed By |
|---|---|
| Coughing or sneezing | Birth (spread from an infected mother to her baby during birth) |
| Hugging and kissing or other casual contact | Direct contact with the blood or open sores of an infected person |
| Sharing food, drinks, or eating utensils | Improperly sterilized equipment used during manicures and pedicures; medical or dental procedures; and tattoos and body piercing |
| Touching or shaking hands | Sex with an infected partner |
| Using toilet seats | Sharing needles, syringes, or other drug-injection equipment |
| Sharing personal hygiene items with an infected person such as nail clippers, razors, or toothbrushes |
Symptoms
What happens when you get hepatitis B depends largely on the age when you’re infected and how well your immune system copes with the virus.
You may have hepatitis B for years and never have any symptoms. You can still spread the virus to others even if you don’t have symptoms.
Acute Hepatitis B Symptoms and Complications
If you’re infected as an adult, you may have a brief illness with mild or moderate symptoms such as:
- abdominal discomfort
- dark urine
- fatigue (feeling tired all the time)
- jaundice (yellowing of the eyes and skin)
- loss of appetite (not feeling hungry)
If you’re infected as an adult, you have a 99% chance of clearing the infection and developing lifelong protection against the virus. The acute infection rarely leads to severe illness that requires a liver transplant (less than 1% of cases).
Chronic Hepatitis B Symptoms and Complications
Most babies and children exposed to the hepatitis B virus never have signs or symptoms. Unfortunately, they’re more likely to become carriers of hepatitis B for life because their immune system is unable to clear the virus from their body. In these cases, their chronic infection is often not detected until much later in life when:
- they’re screened because they come from an area where the virus is common or
- they become seriously ill with liver disease as adults.
Chronic hepatitis B goes through different phases that show how well your body’s coping with the virus. Most people have an inactive disease and stay healthy, but one in four will have an active disease. If untreated, this may lead to cirrhosis and/or liver failure. Liver cancer is also a risk for all patients with chronic hepatitis B. Therefore, screening for hepatitis B is important.
People who are healthy with an inactive disease are still at risk of the virus becoming active again. This can happen spontaneously, or when their immune system is weakened by other viral infections or medicines such as chemotherapy, especially corticosteroids.
Diagnosis
To confirm if you have hepatitis B, you’ll need lab tests such as the following:
| Lab Test | If This Test is Positive, it Means: |
|---|---|
| Hepatitis B Surface Antibody (Anti-HBs or HBsAb) | You have antibodies against hepatitis B and are protected from getting the disease. You were either vaccinated against hepatitis B or exposed to it at some point in your life. |
| Hepatitis B Core Antibody (Anti-HBc) | You’ve been exposed to hepatitis B and have developed an antibody to just one part of the virus. This antibody does not give you immunity. You need more tests to find out if you have the disease. |
| Hepatitis B Surface Antigen (HBsAg) | You currently have a hepatitis B infection. You can spread the virus to others. |
| Hepatitis B e Antigen (HBeAg) | You may have very active hepatitis B and should be followed closely by your doctor. You may also need to take hepatitis B medications. You may be very contagious to others. |
Treatment
Not all people with hepatitis B need treatment. Choosing the right time for treatment is not a simple decision. It’s based on the results of your lab tests, your age, and the amount of scarring and inflammation in your liver. A liver biopsy may also be required. If you have cirrhosis, you might be a candidate for treatment as well.
You will definitely need treatment if you have an active disease that causes a lot of damage to your liver. You’ll also need treatment if you’re going to take medications that weaken your immune system.
When and how to treat your hepatitis B are decisions between you and your doctor. Availability of medications may also vary based on health insurance plans.
Even if you don’t need treatment for your hepatitis B, you will need regular screening for liver cancer. This is done with abdominal ultrasound every 6 months. Cancers detected early may be cured. This screening needs to start at age 40 in males, age 50 in females, and at age 20 in those of African birth.
Types of Treatment Available
If you know you’ve been exposed to the hepatitis B virus in the last seven days, you can receive an injection of hepatitis B immune globulin. This might prevent you from developing the disease. Besides this, there is no treatment for acute hepatitis B.
There are two types of treatment for chronic hepatitis B:
- Interferon. This is a medication given by needle. It’s rarely used due to its many side effects and the effective antiviral medicines noted below.
- Antiviral medicines. These are oral medications (taken by mouth) and include adefovir, entecavir, lamivudine, telbivudine, and tenofovir. Hepatitis B can develop resistance to these drugs. To avoid this, remember to take your medications every day. Entecavir and tenofovir are the best choices with only a very small chance of the virus becoming resistant.
These medications can’t cure hepatitis B, but they do control the virus so that further damage to your liver can be prevented.
Taking Medications and Monitoring Your Hepatitis B
Your doctor will recommend hepatitis B medications if you have liver inflammation and a very active virus. These are indicated by a high viral load, which means a high amount of hepatitis B virus in your blood. You’ll also have a high level of ALT, one of the liver enzymes that helps the liver do its work. A high ALT level indicates the liver is being damaged.
Hepatitis B medications are important during phases of prolonged liver inflammation. Your healthcare providers will track the phase of your hepatitis B by the results of your lab tests. Because infected people go through various phases of hepatitis B, it’s recommended that they have lab tests regularly.
If you’re on hepatitis B medications, your healthcare providers will monitor you closely. You’ll need lab tests every 3 to 6 months to monitor your viral load and ALT level. You’ll also need other tests such as hepatitis B e antigen (HBeAg), and you’ll need to see your doctor regularly.
Q&A

No. Even if treatment is successful, it doesn’t completely get rid of the hepatitis B virus. However, successful treatment can stop the virus from multiplying. It can also stop liver inflammation. Stopping the inflammation will reduce the chance of developing cirrhosis or liver cancer.
That being said, 1 – 3% of people will completely clear the virus from their body each year. This can occur on or off treatment.
To avoid getting the hepatitis B virus or spreading it to others:
- Use a condom when you have sex.
- Don’t share needles.
- Wear latex or plastic gloves if you have to touch others’ blood.
- Don’t share toothbrushes or razors.
- Don’t get a tattoo. Or make sure the needles have been cleaned properly and are sterile.
- Babies of mothers with chronic hepatitis B must receive both a vaccine and a special hepatitis B immune globulin (HBIG) at birth.
References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References:
