The best way to describe autoimmune hepatitis is to break down the term “autoimmune.” Autoimmune refers to the body’s own immune system attacking another part of the body. In this case, the immune system attacks the liver and causes liver inflammation.
Autoimmune hepatitis is not contagious. Also, it’s not considered an inherited disease. But a tendency to autoimmune diseases may run in some families.
Causes
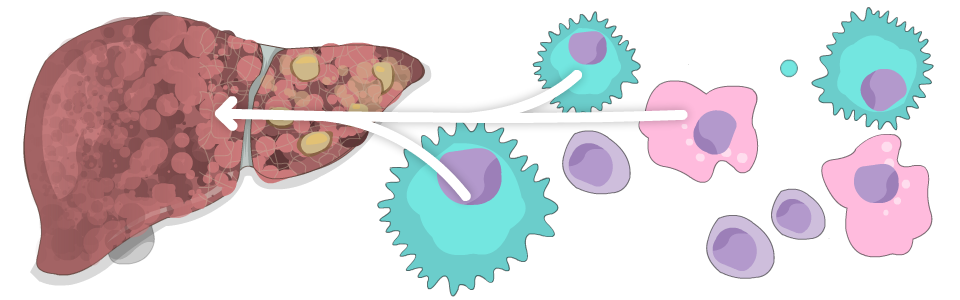
We don’t yet know exactly why or how the body’s immune system attacks its own liver. But we do know it happens because of a mistake made by certain types of white blood cells, the cells that fight infections. It appears that white blood cells misread liver cells as harmful foreign substances and attack them. This causes liver inflammation. With time, this ongoing inflammation might lead to fibrosis (scarring of the liver) and eventually cirrhosis (severe scarring of the liver).
Several other things can cause identical patterns of liver damage. These include viruses such as hepatitis B and hepatitis C, certain types of drugs, and an overload of certain metals in the liver such as copper and iron. There are also other causes that are very rare.
Symptoms
In many people, there are no symptoms at all. They feel perfectly healthy. Other people may experience:
- aches or pains in the muscles or joints
- decreased appetite
- drowsiness
- fatigue
- jaundice (yellowing of the eyes and skin)
Diagnosis
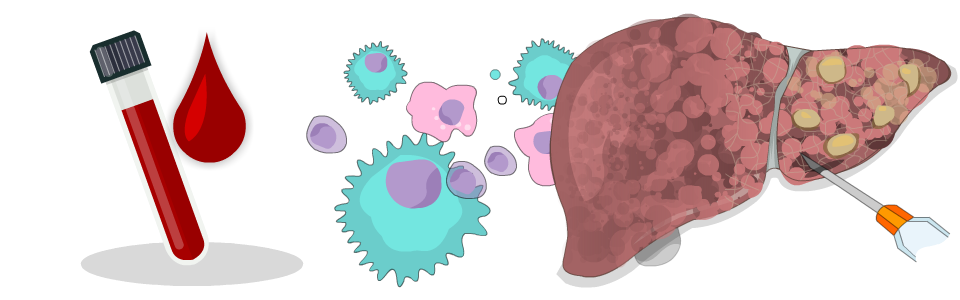
Autoimmune hepatitis may be detected with a series of blood tests.
The initial clue from blood tests is high levels of ALT and AST, which are two enzymes made by the liver. However, ALT and AST levels go up in many liver diseases or conditions, so the next step to diagnose autoimmune hepatitis is to measure specific antibodies directed against parts of different cells. These are called autoantibodies.
Your doctor will also examine you and may find signs such as a large liver and jaundice.
Finally, a liver biopsy is usually necessary to confirm the diagnosis, determine the extent of liver damage, and ensure there aren’t co-existing liver conditions.
Treatment
Since we don’t know exactly what causes autoimmune hepatitis, we don’t yet have a medical cure. But we do have effective treatments.
If the disease is mild or inactive, you might not need any type of treatment. When medications are needed, corticosteroids are the first treatment of choice. Corticosteroids are different from anabolic steroids, which are used to build muscle mass. Corticosteroids such as prednisone are potent anti-inflammatory drugs. They reduce inflammation throughout the body, including the liver. There are side effects, however, so your doctor will try to use the smallest amount possible to control the disease.
Your doctor may also prescribe other anti-inflammatory drugs such as azathioprine, methotrexate, or mycophenolate mofetil. All these drugs have side effects your doctor will explain in detail. These can also help to limit the dose of corticosteroids you require.
After drugs have reduced the initial inflammation caused by autoimmune hepatitis, about 90% of people need ongoing treatment to stay in remission. This treatment is usually azathioprine. About 10% don’t need ongoing treatment. They remain in remission with no symptoms and no active inflammation in the liver for many years. But they do require monitoring with simple blood tests.
Since the intensity of the disease goes up and down, some people suffer from relapses—even those who have been receiving ongoing treatment. Relapses are usually treated by a temporary course of corticosteroids.
Note: This section was adapted (with permission) from content on the website of the Canadian Liver Foundation.
References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References:
