Top tips:
- Available data on this topic is predominantly non-randomized and observational. Guidance statements are consistent with expert documents from AASLD (PMID 33219529, Baveno VII (PMID 35120736) and PMID 33930474). Consult specialist on-call for most cases of PVT in cirrhosis.
- The main potentially lethal consequences of PVT in cirrhosis are variceal hemorrhage and intestinal ischemia/necrosis
- Doppler ultrasound is the first-line evaluation for the diagnosis of portal vein thrombosis (PVT). Perform an Ultrasound doppler to evaluate for PVT in all patients with (i) a new diagnosis of cirrhosis, (ii) onset of portal hypertension, (iii) hepatic decompensation.
- CT or MRI should be used to confirm the diagnosis, to exclude tumor thrombus and assess extension into the mesenteric veins
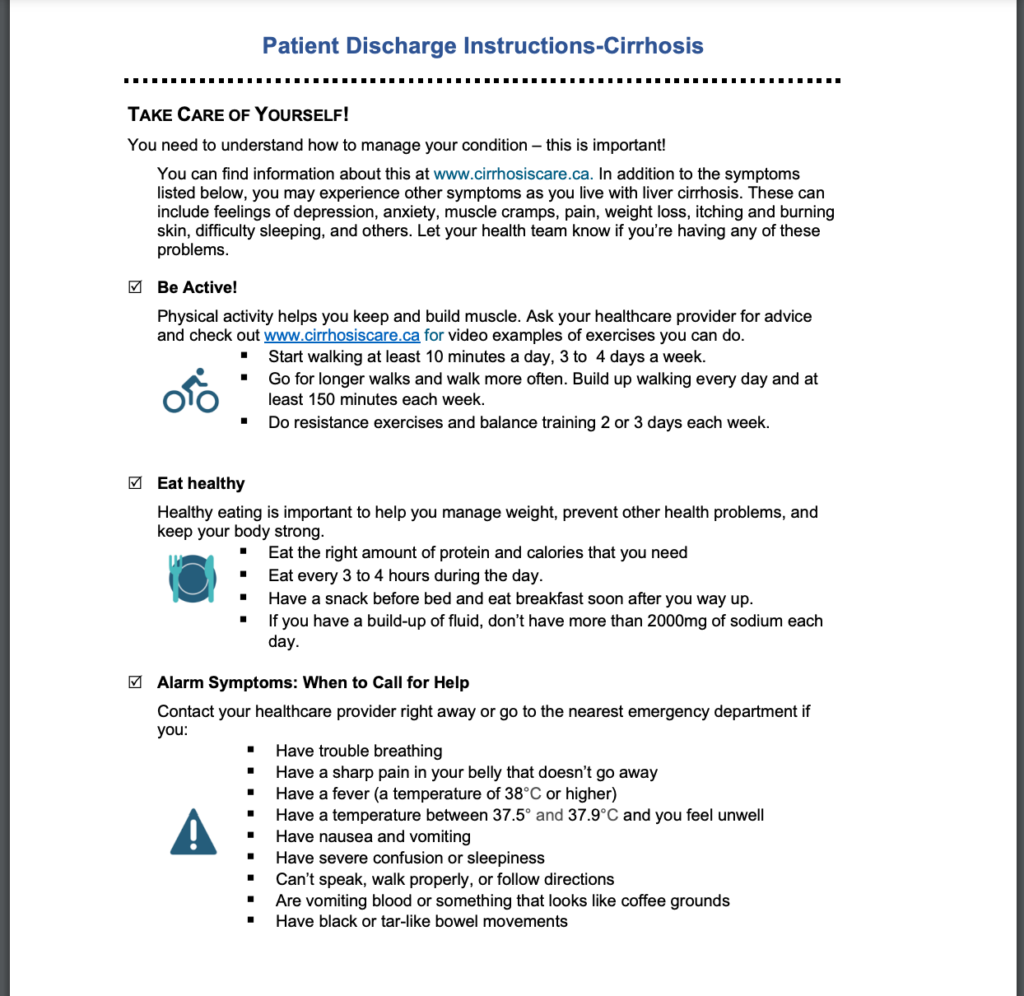
- In patients with chronic PVT who meet indication for anticoagulation, assess for high-risk varices with endoscopy. If high risk varices are present, non-selective beta-blockers are suggested for the primary prevention of variceal bleeding.
- In cirrhosis, it can be challenging to determine the chronicity of PVT because portal cavernoma is less frequent.
- The goal of PVT therapy in cirrhosis is to avoid progression of the clot that predisposes to worsening portal hypertension, impacts the ability to perform a liver transplant, or liver transplant outcomes.
- Variceal prophylaxis should be carried out as per AASLD and Baveno variceal guidelines. Link to varices page
- See algorithm below for indications for anticoagulation.
- HCC related tumor thrombus does not benefit from anticoagulation
- Continue anticoagulation until recanalization, and for at least 6 months. Consider longer term anticoagulation even after recanalization in all patients, especially those with SMV involvement, a history of intestinal ischemia or thrombophilic state or if the patient is a liver transplant candidate.
- If anticoagulation is stopped, check PV patency within 3 months after stopping, as re-thrombosis rates are high – up to 38% by 4 months.
General Cirrhosis Admission and Discharge Order Sets
*Add specific panels to general admission orders as appropriate*
For adults with cirrhosis requiring hospital admission
Cirrhosis Adult Admission Orders
For adults with cirrhosis requiring hospital discharge
Cirrhosis Adult Discharge Orders

Thank you to Dr. Garcia-Tsao for your efforts creating the content on this page!
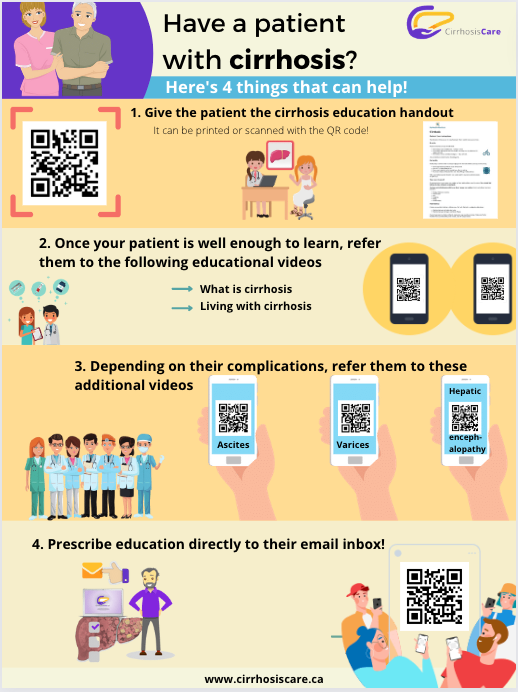
Patient materials:
You can direct patients to the following:
Portal hypertension
Downloadable content:
You can download these to print or view offline:
EASL Guidelines for decompensated cirrhosis
References:
This section was adapted from content using the following evidence based resources in combination with expert consensus. The presented information is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient’s care.
Authors: Dr. Vladimir Marquez, Dr. Guadalupe Garcia-Tsao, Dr. Wayne Bai, Dr. Puneeta Tandon
References:
- Simonetto DA, Singal AK, Garcia-Tsao G, Caldwell SH, Ahn J, Kamath PS. ACG Clinical Guideline: Disorders of the Hepatic and Mesenteric Circulation. Am J Gastroenterol 2020 Jan;115(1):18-40. PMID 31895720
- Francoz C, Valla D, Durand F. Portal vein thrombosis, cirrhosis, and liver transplantation. J Hepatol 2012;57:203–12. PMID 22446690
- Nery F, Chevret S, Condat B, et al. Causes and consequences of portal vein thrombosis in 1,243 patients with cirrhosis: Results of a longitudinal study. Hepatology 2015;61:660–7.PMID 25284616
- Yerdel MA, Gunson B, Mirza D, et al. Portal vein thrombosis in adults undergoing liver transplantation: Risk factors, screening, management, and outcome. Transplantation 2000;69:1873–81.PMID 10830225
- Kreuziger LB, Ageno W, Lee A. Management of incidental splanchnic vein thrombosis in cancer patients. Hematology Am Soc Hematol Educ Program 2014;2014:318–320. doi: 10.1182/asheducation-2014.1.318.PMID 25696872
Last reviewed September 26, 2022