Session 1: Alcohol use disorder 101
Learning objectives:
By the end of the session, participants will be able to:
1. Explain the biological process of alcohol use disorder as a brain disease
2. Review existing literature on healthcare practitioner attitudes towards patients with alcohol use disorder
3. Describe the multi-system consequences of alcohol use disorder
4. Manage patients with alcohol withdrawal
Pre-recorded presentation
Additional resources
WHO Alcohol Brief Intervention Training Manual for Primary Care
Motivational Interviewing – Alcohol Video
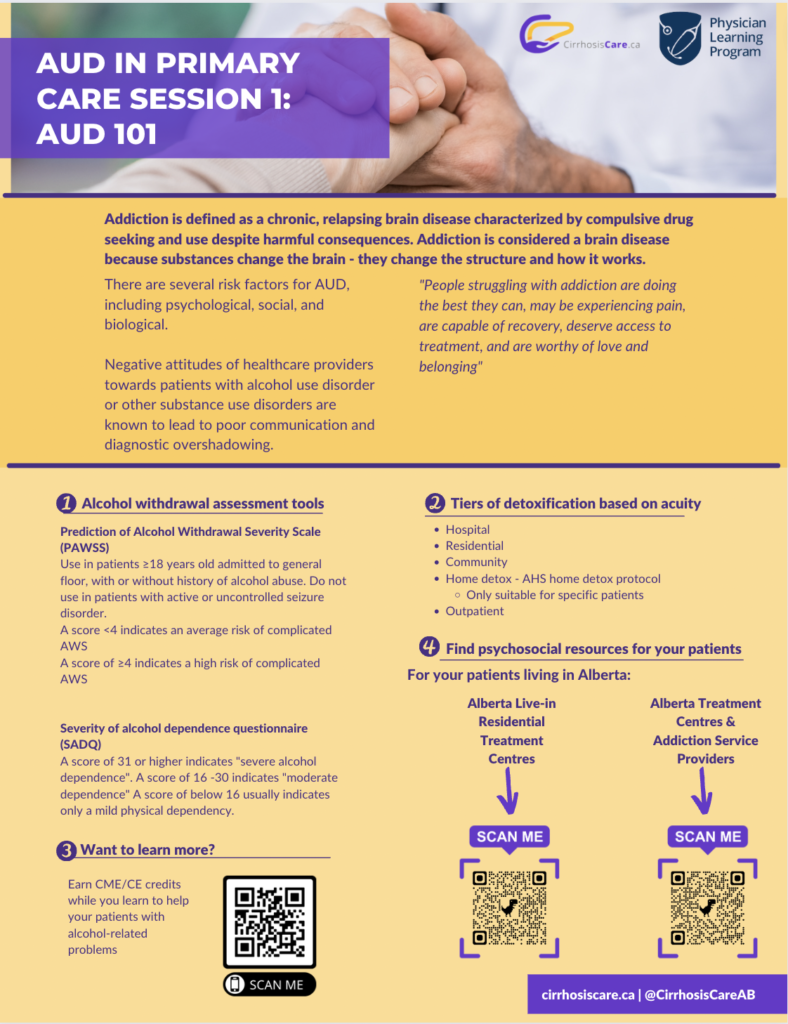
Severity of Alcohol Dependence Questionnaire (SADQ)
Prediction of Alcohol Withdrawal Severity Scale (PAWSS)
Canadian Resources
Canada’s Low Risk Drinking Guidelines
Guidelines for Healthcare Providers to Promote Low Risk Drinking Guidelines
Alcohol in Canada: Canadian Centre on Substance Use and Addiction
Substance Use Treatment Centres for First Nations and Inuit
Practical Approach to Substance Use Disorders for the Family Physicians
Canadian Alcohol Use Disorder Society
Alberta Resources
Alberta Addiction Treatment Directory
Recovery Access Alberta: Treatment directory for patients and providers
Alcoholics Anonymous Meetings Alberta
Recovery Dharma Alberta: Using Buddhist Practices
United States Resources
Substance Use and Mental Health Services Administration
National Institute on Drug Abuse
Further Reading
Healthcare Teamwork: Interprofessional Practice and Education
Beyond the Checklist: What Else Healthcare Can Learn from Aviation Teamwork and Safety
References
-
- Ries, R., Ovid Technologies, Inc., & R2 Online Library. (2009).Principles of addiction medicine.Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins.
- American Society of Addiction Medicine (2019). Definition of addiction. Rockville, MD.
- Gage, S. H., & Sumnall, H. R. (2019). Rat Park: How a rat paradise changed the narrative of addiction. Addiction, 114(5), 917–922.https://doi.org/10.1111/add.14481
- O’Connor, P. G., Sokol, R. J., & D’Onofrio, G. (2014). Addiction medicine: the birth of a new discipline.JAMA internal medicine. 174(11), 1717-1718.
- Herron, A., & Brennan, T. K. (2019). The ASAM essentials of addiction medicine. Lippincott Williams & Wilkins.
- “The Biopsychosocial Model Approach” (PDF).Rochester University. Rochester University. Retrieved 18 April 2019.
- Borrell-Carrió, F., Suchman, A. L., & Epstein, R. M. (2004). The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Annals of family medicine 2(6), 576–582. https://doi.org/10.1370/afm.245
- Canadian Centre on Substance Use and Addiction. (2019). Alcohol. Ottawa: Author.
- Varin M, Palladino Elia, Hill MacEachern K, Belzak L, Baker MM. Prevalence of alcohol use among women of reproductive age in Canada. Health Promot Chronic Dis Prev Can. 2021;41(9):267-71. https://doi.org/10.24095/hpcdp.41.9.04
- University of Victoria, Canadian Institute for Substance Use Research. British Columbia Alcohol
- van Boekel, L. C., Brouwers, E. P., van Weeghel, J., & Garretsen, H. F. (2013). Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review.Drug and alcohol dependence 131(1-2), 23–35.
- Palmer, R. H., Young, S. E., Hopfer, C. J., Corley, R. P., Stallings, M. C., Crowley, T. J., & Hewitt, J. K. (2009). Developmental epidemiology of drug use and abuse in adolescence and young adulthood: Evidence of generalized risk. Drug and alcohol dependence 102(1-3), 78–87.
- Thornicroft, G., Rose, D., Kassam, A., & Sartorius, N. (2007). Stigma: ignorance, prejudice or discrimination?. The British journal of psychiatry : the journal of mental science 190–193. https://doi.org/10.1192/bjp.bp.106.025791
- Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: a neurocircuitry analysis. The lancet. Psychiatry 3(8), 760–773. https://doi.org/10.1016/S2215-0366(16)00104-8
- Mattoo, S. K., Prasad, S., & Ghosh, A. (2018). Brief intervention in substance use disorders. Indian journal of psychiatry 60(Suppl 4), S466–S472. https://doi.org/10.4103/0019-5545.224352
- Bertholet, N., Daeppen, J. B., Wietlisbach, V., Fleming, M., & Burnand, B. (2005). Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Archives of internal medicine 165(9), 986–995. https://doi.org/10.1001/archinte.165.9.986
-
Stockwell, T., Sitharthan, T., McGrath, D., & Lang, E. (1994). The measurement of alcohol dependence and impaired control in community samples. Addiction (Abingdon, England), 89(2), 167–174. https://doi.org/10.1111/j.1360-0443.1994.tb00875.x
- Cotter TG, Ayoub F, King AC, Reddy KG, Charlton M. Practice Habits, Knowledge, and Attitudes of Hepatologists to Alcohol Use Disorder Medication: Sobering Gaps and Opportunities. Transplantation Direct. 2020;6(10):e603. doi:10.1097/txd.0000000000001054.